What is Vitiligo?

Vitiligo’s emotional impact
August 10, 2017
World Vitiligo Day
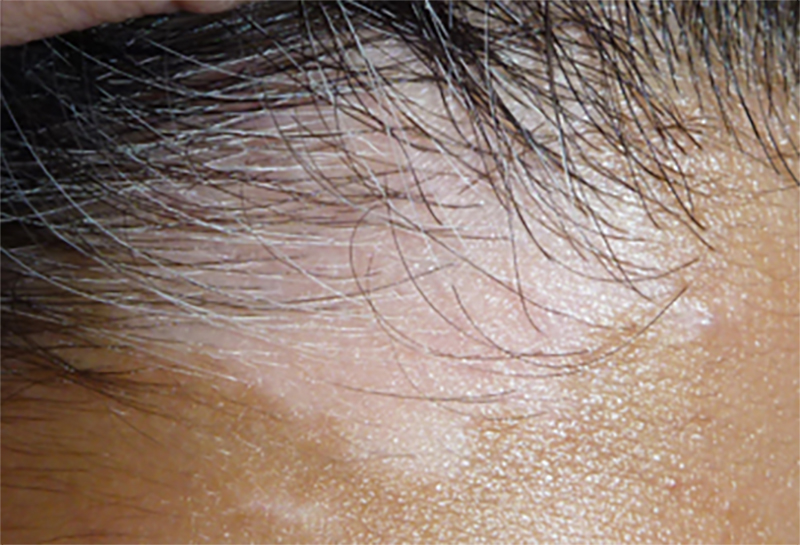
June 24, 2019Vitiligo is regarded as an acquired pigmentary disorder of the skin and mucous membranes resulting in white macules (a flat, distinct, discoloured area of skin less than 5 millimetres (mm) wide) and patches (greater than 5-10 millimetres (mm) wide). These white macules and patches are due to the destruction and loss of melanocytes. Melanocytes are melanin-producing cells located in the bottom layer (the stratum basale) of the skin’s epidermis. Melanin is the pigment that gives human skin, hair, and eyes their colour. May also be called leukoderma which is a generic term applied to any pigmentary loss.
Vitiligo affects approximately 0.5 % to 1 % of the population worldwide, with rates as high as 8·8% in India. While the condition may be more noticeable in dark-skinned people, adults and children of both sexes are equally affected, although women and girls often present for treatment more frequently, possibly because of the greater negative social effects for affected women and girls than for men and boys. The average age of onset of vitiligo is in the mid-twenties, but it can appear at any age.

Gill L. et al; High Prevalence of Autoimmune Disease Observed in a Cohort of Patients with Vitiligo; https://www.aad.org/eposters/Submissions/getFile.aspx?id=1068&type=sub
About 15 to 25 % of people with vitiligo are also affected by at least one other autoimmune disorder, particularly autoimmune thyroid disease (Hashimoto’s thyroiditis), rheumatoid arthritis, type 1 diabetes, psoriasis, pernicious anaemia, Addison disease, or systemic lupus erythematosus. 1, 2, 3, 4
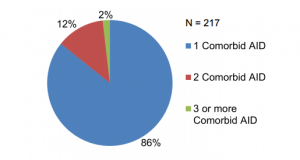
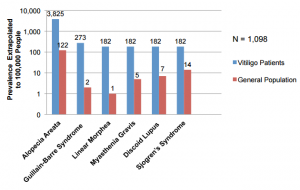

Gill L. et al; High Prevalence of Autoimmune Disease Observed in a Cohort of Patients with Vitiligo; https://www.aad.org/eposters/Submissions/getFile.aspx?id=1068&type=sub
Both genetic and non-genetic factors are involved in the onset of vitiligo and although the exact mechanism causing the destruction of the melanocytes remains unknown.
Researchers hypothese that genetic, immunological, neurohormonal, cytotoxic, biochemical and oxidative stress are involved and the exact triggers of the condition vary widely patient by patient, thus making it difficult to conclusively define the primary cause. However, given that autoimmune diseases typically involve interactions between genetic risk factors and environmental triggering factors, the autoimmune theory seems to be the most plausible.
In vitiligo, after the genetic component (approx. 20 -30% have at least one affected first-degree relative) is taken into consideration, the triggering factors are considered to be environmental i.e. poor nutrition, emotional stress, trauma (Koebner Phenomenon), drugs, infections, exposure to the sun and chemicals, toxins and sepsis.
In most studies vitiligo is broadly classified into four types.4
The four types are:-
- Non-segmental vitiligo (NSV) – accounts for 70% of vitiligo patients
- Segmental vitiligo (SV) – accounts for 30% vitiligo patients
- Mixed NSV and SV – Approx. 6% of the above NSV patients will present with a SV lesion elsewhere on the body while approx. 19% of above SV patients had SV in combination with other types of vitiligo and 10% of these progressed to NSV.
- Unclassifiable types e.g., focal, multifocal asymmetrical non-segmental and mucosal at one site.
Non-segmental vitiligo develops at all ages, but usually occurs in young people between the ages of 10 years and 30 years, with 87% of cases presenting before age 30 years and 41% before age10 years. Non-segmental vitiligo lesions typically have a bilateral distribution affecting both the face, hands and feet (acrofacial), or can be scattered symmetrically over the entire body, evolving over time. Non-segmental vitiligo can initially present in an acrofacial distribution, but over time can progress to the generalised or universal form. 1, 2, 3, 5
The terms ‘contact’ or ‘occupational vitiligo’(CV) has been used to describe a distinct form of vitiligo induced by exposure to certain chemicals in the workplace or at home. However, the precise definition of CV is unclear. Indeed, although the cutaneous depigmentation may be limited to the areas exposed to chemicals, it may extend progressively from the initial site of chemical contact to the whole body, leading to typical NSV 5
SV is often associated with the occurrence of white hair (i.e. poliosis, leukotrichia) in lesional skin.
Poliosis and leukotrichia are due to lack of melanin (pigment) in the hair shafts of the affected area. Poliosis (cluster of depigmented hair) is not restricted/specific to vitiligo. It is most often seen in scalp hair, but may also affect eyebrows, eyelashes or other sites. 6
SV tends to involve the hair compartment soon after onset compared to NSV. One study reported that poliosis was found in 49% of 208 patients with SV. 6
Hearing loss and loss of pigmentation of the iris (retinitis pigmentosa) although rare, may also be involved. The emotional impact of vitiligo cannot be understated. To this end we have prepared a separate blog dedicated to this critical topic.
REFERENCES
- Prashiela Manga et al.; REVIEW Recent advances in understanding vitiligo; F1000Research 2016, 5(F1000 Faculty Rev):2234 Last updated: 25 DEC 2016
- Genetics Home Reference: https://ghr.nlm.nih.gov/condition/vitiligo; USA U.S. National Library of Medicine National Institutes of Health
- Ezzedine K. et al.; Vitiligo; Seminar; www.thelancet.com Published online January 15, 2015 http://dx.doi.org/10.1016/S0140-6736(14)60763-7
- Vijayalakshmi B.; A Clinical Study of Vitiligo and Associated Autoimmune Disorders – A Retrospective Study.; Annals of International Medical and Dental Research, Vol (3), Issue (2)
- Ezzedine K. et al.; Revised classification/nomenclature of vitiligo and related issues: the Vitiligo Global Issues Consensus Conference; Pigment Cell Melanoma Res. 2012 May; 25(3): E1–13.; doi: 10.1111/j.1755-148X.2012.00997.x
- Ji-Hye Park and Dong-Youn Lee; Segmental Vitiligo; Vitiligo – Management and Therapy; Chapter 7.; DOI: 10.5772/38936 · Source: InTech
[/vc_column_text][/vc_column][/vc_row]